| Jae Keun Oh | 6 Articles |
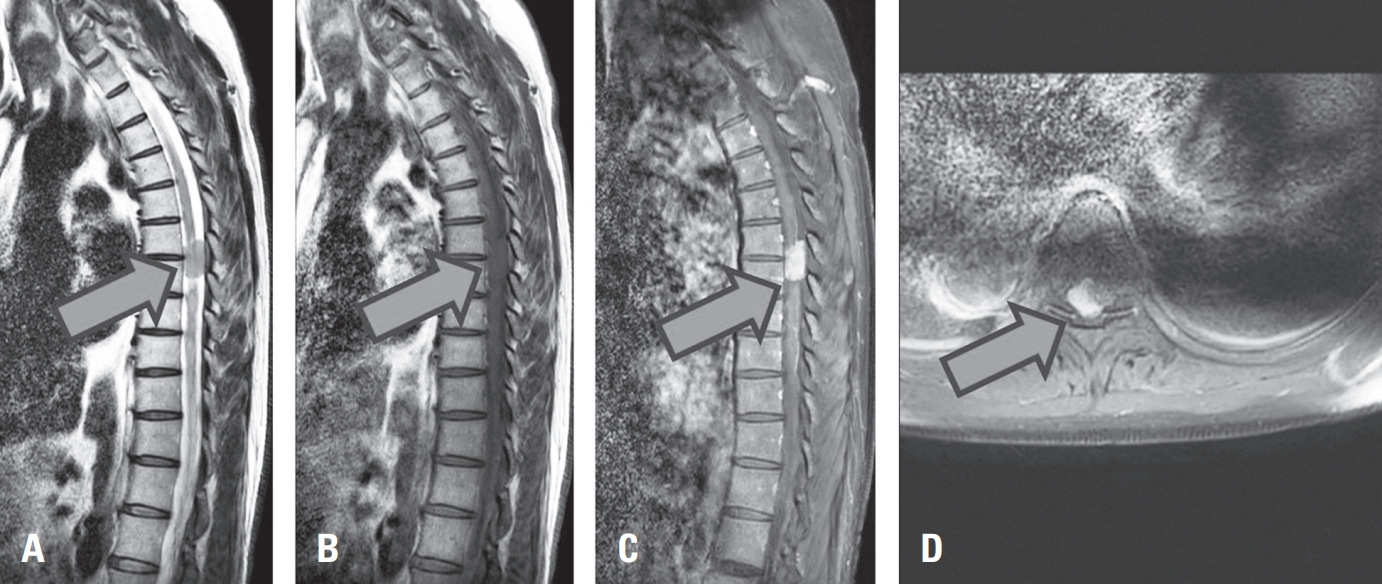
Primary glioblastoma of the spinal cord is a rare and aggressive tumor, comprising less than 1.5% of spinal neoplasms. It typically affects young adult males and arises in the cervical or thoracic regions. We report an unusual case of intradural extramedullary spinal glioblastoma in a 62-year-old man with prior lymphoma in remission. The patient presented with a 7-month history of progressive lower limb weakness, numbness, and radiating pain. MRI revealed a contrast-enhancing mass at the T6–7 level, initially suspected as lymphoma. Surgical resection via total laminectomy was performed, and en-bloc tumor removal achieved. Histopathological analysis confirmed WHO grade IV glioblastoma, IDH-wildtype, without Histone H3 mutation. This case highlights an atypical radiologic and anatomical presentation, complicating preoperative diagnosis. Histopathologic and molecular studies were essential for confirmation. Postoperative treatment included adjuvant radiotherapy and temozolomide, though their efficacy remains uncertain in spinal glioblastoma due to limited evidence and spinal cord radiosensitivity. Early biopsy and a multimodal diagnostic approach are critical for managing rare spinal tumors presenting with nonspecific clinical and imaging features.
Advanced imaging technologies have revolutionized the diagnosis and management of spinal pathologies by providing superior precision and efficiency. Modalities such as PET-CT, SPECT, diffusion tensor imaging (DTI), and magnetic resonance spectroscopy (MRS) offer unique insights into the metabolic, structural, and functional aspects of spinal diseases, enabling better differentiation of lesions, improved surgical planning, and early detection of pathological changes. Furthermore, the integration of artificial intelligence (AI) has enhanced imaging workflows by enabling automated analysis, prediction of clinical outcomes, and segmentation of spinal structures. Despite these advancements, challenges such as technical limitations, high costs, and ethical concerns, including issues of data privacy and AI-generated inaccuracies, hinder widespread adoption. This review explores the clinical applications, limitations, and future directions of these emerging technologies, highlighting the need for multidisciplinary collaboration and large-scale research to standardize protocols and optimize patient outcomes. The seamless integration of advanced imaging and AI represents a transformative potential for improving diagnostic accuracy and treatment efficacy in spinal care.
After posterior cervical arthrodesis, many problems can arise, including adjacent segment degeneration and the related adjacent segment disease (ASD). As indicated by studies on the causes of ASD, posterior cervical arthrodesis can produce biomechanical and kinematic changes in adjacent unfused segments due to inappropriate forces.
Several studies have been conducted to determine the appropriate lowest instrumented vertebra, specifically regarding whether to cross the cervicothoracic junction via extension of long-segment posterior cervical fusion. We searched for relevant articles in electronic databases including PubMed, the Cochrane Registry, Embase, and Ovid.
Five meta-analyses were reviewed on this topic. Among these, Goyal et al. (2019), Rajjoub et al. (2022), and Chang et al. (2022) argued that ending instrumentation at the cervical level was associated with higher rates of ASD and reoperation. However, Truumees et al. (2022) and Coban et al. (2022) found no statistically significant differences between cases of instrumentation ending at the cervical and thoracic levels in the rates of ASD and requirement of revision surgery. Cervicothoracic junction breakage is a known possibility after cervical spine surgery because of the anatomical fragility of the junction. Terminating at the thoracic level reduces the stress on the cervicothoracic junction, thereby decreasing complications such as cervicothoracic junction breakage and lowering the frequency of reoperation. Based on the findings published to date, instrumentation across the cervicothoracic junction can be reasonably recommended in cases of multilevel posterior cervical fusion based on the lower reoperation and higher fusion rate.
Purpose
of Study: Purpose of this study is to summarize the technique of UBE surgery in lumbar interbody fusion and review the clinical outcomes and complications of UBE surgery in lumbar interbody fusion. Materials and Methods Medical databases were searched for the key words of unilateral biportal endoscopic surgery and lumbar spinal stenosis using PubMed from 2005 to the present. Conclusion UBE spinal surgery is a new technique that can be a feasible alternative and an effective treatment modality for spinal degenerative diseases and can achieve the necessary surgical skills for experienced microscopic surgeons, which is still expanding the indications for lumbar spinal surgery.
Purpose
To analyze the serial change of the cervical saggital alignment especially cobb angle from immediately post operation to 3 month of post operation, and evaluate the effect of anatomically designed pillow to restore cervical lordosis. Materials and Methods cervical cobb angle (C2-C7) was measured in 38 patients whose radiographs at immediately post op, post op 1mo and post op 3mo were completely equipped. The patient group consisted of 10 patients in the general pillow group, 19 patients in the cervical pillow group, and 9 patients in the Philadelphia orthosis group. Results There was no statistically significant difference between the two groups using any pillow and the group using Philadelphia orthosis. Among them, patients who used anatomically designed pillow for 1 month to 3 months postoperatively were more likely to have lordotic change than the other patients, though it was not statistically significant. Conclusion The use of a cervical orthosis until the first month after the operation and subsequently anatomically degsined pillow for up to 3 months may be considered as a way to maintain lordotic curvature and prevent kyphotic changes.
Purpose
of study: The purpose of this study is to understand the biomechanics of interspinous devices in lumbar spinal surgery and to review the effectiveness of the devices for lumbar spinal stenosis through recent related articles. Materials and Methods Medical databases were searched for the key words of interspinous device and lumbar spinal stenosis using PubMed from 2010 to the present. Results Several studies have shown sustained symptomatic improvements after interspinous device insertion. However, most of the prospective, randomized, double-blinded studies have shown that it is not superior to conventional laminectomy from a statistical perspective. Furthermore, interspinous device insertion has been shown to have a higher reoperation rate and to be less cost effective. Conclusions A large prospective cohort study with a longer follow-up period comparing decompressive surgery alone versus interspinous device insertion for the treatment of lumbar spinal stenosis is needed to conclusively determine whether the interspinous device is beneficial.
|
|

