Abstract
-
Purpose
To report an uncommon case of Opalski syndrome following traumatic C4–C5 facet dislocation with vertebral artery dissection, and to discuss its diagnostic and therapeutic implications.
-
Materials and Methods
A 60-year-old woman presented after a motor vehicle collision with bilateral upper limb weakness. Cervical X-ray, CT, MRI, and CT angiography revealed C4–C5 facet dislocation and left vertebral artery occlusion. Urgent anterior cervical discectomy and fusion were performed, and the postoperative course was monitored.
-
Results
Immediate postoperative improvement to 4/5 strength in both arms was noted; however, new left facial numbness appeared at 12 hours and left lower limb weakness with gait ataxia at 48 hours. Brain MRI confirmed left lateral medullary infarction, and aspirin therapy was initiated. At one month, left arm strength recovered to 4/5, but ataxia persisted.
-
Conclusions
In cervical trauma patients with C4–C5 facet dislocation and vertebral artery injury on initial imaging, the possibility of delayed lateral medullary infarction—particularly Opalski syndrome—should be considered. Prompt brainstem imaging and tailored antithrombotic therapy are essential when new neurologic deficits arise.
-
Keywords: Opalski syndrome, Vertebral artery dissection, Cervical facet dislocation, Lateral medullary syndrome
Abstract
-
목적
외상성 C4-C5 후관절 탈구로 인한 척추동맥 박리 후 Opalski 증후군이 발생한 드문 사례를 보고하고, 진단 및 치료적 시사점을 제시하고자 하였다.
-
대상 및 방법
60세 여성이 교통사고 후 양측 상지 근력 약화로 내원하였다. 영상검사(경추 X-ray, CT, MRI, CT-angio)에서 C4-C5 후관절 탈구와 좌측 척추동맥 폐색이 확인되어 응급 전방 추간판제거술 및 유합술을 시행하고 경과를 관찰하였다.
-
결과
수술 직후 상지 근력은 양측 모두 4/5로 호전되었으나, 12시간 후 좌측 안면 무감각, 48시간 후 좌측 하지 약화 및 보행 실조가 발생하였다. Brain MRI에서 좌측 연수측방 경색이 확인되어 아스피린을 투여하였으며, 1개월 후 상지 근력은 4/5로 회복되었으나 실조는 지속되었다.
-
결론
C4-C5 후관절 탈구 및 초기 영상에서 척추동맥 손상이 확인된 경추외상 환자에서는 지연성 lateral medullary infarction, 특히 Opalski 증후군 가능성을 고려하여 새로운 신경학적 증상 발생 시 신속한 뇌간 영상 검사 및 적절한 항혈전 치료가 필요하다.
-
색인 단어: 연수측방증후군, Opalski 증후군, 척추동맥 박리, 경추 후관절 탈구
Introduction
Motor deficits following cervical spinal injury most commonly manifest as bilateral weakness below the level of the lesion. However, when unilateral paresis develops, alternative mechanisms must be considered.
Opalski syndrome—a rare variant of lateral medullary (Wallenberg) syndrome—is distinguished by the addition of ipsilateral hemiparesis to the classic features of Wallenberg syndrome (trigeminal sensory loss, dysphagia, dysarthria, and Horner’s syndrome). While most reported cases arise from vertebral artery dissection or atherosclerotic disease, the occurrence of Opalski syndrome following traumatic cervical injury remains exceedingly rare.
1)
Here, we present a case of Opalski syndrome in a patient who sustained an unstable C4–C5 fracture with cervical spinal cord injury secondary to a motor vehicle collision, subsequently developing ipsilateral motor weakness. We aim to underscore the diagnostic clues for atypical brainstem ischemic lesions after traumatic cervical injury and to emphasize the importance of early recognition and appropriate management strategies in such cases.
Case Presentation
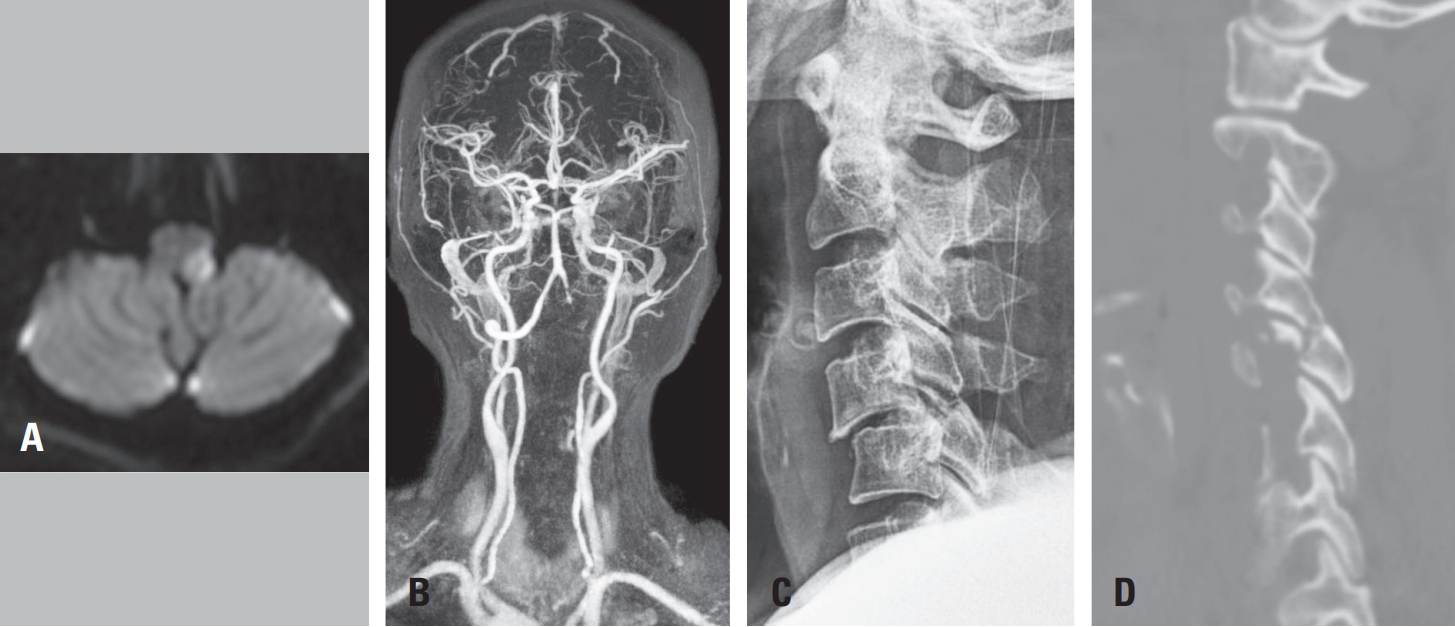
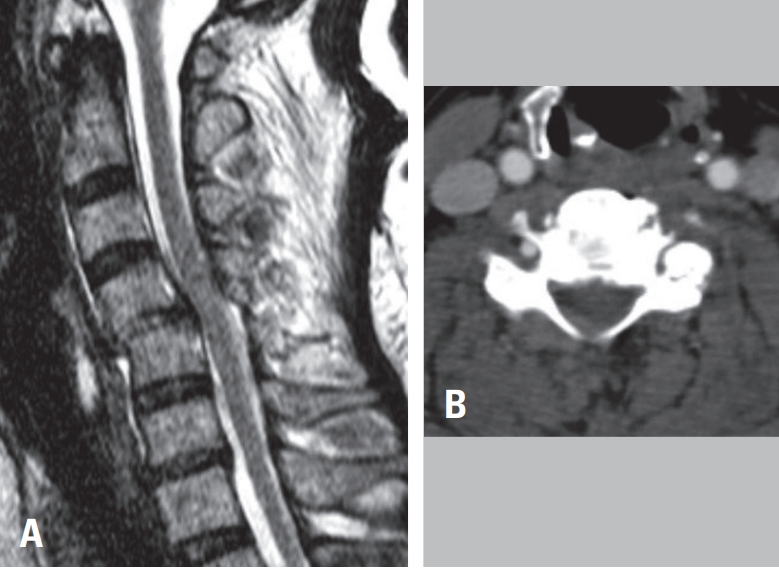
60-year-old woman presented following a motor vehicle collision with notable upper extremity weakness. On examination, motor strength was 2/5 in the left arm and 3/5 in the right arm. Cervical spine radiographs revealed dislocation at the C4–C5 level (
Fig. 1A). Computed tomography demonstrated locking of the left facet joint and subluxation of the right facet joint (
Fig. 1B). Magnetic resonance imaging showed spinal cord compression at C4–C5 with corresponding intramedullary signal change (
Fig. 1C).
To evaluate for vertebral artery injury secondary to facet dislocation, neck CT angiography was performed, confirming occlusion of the left vertebral artery at C4–C5 (
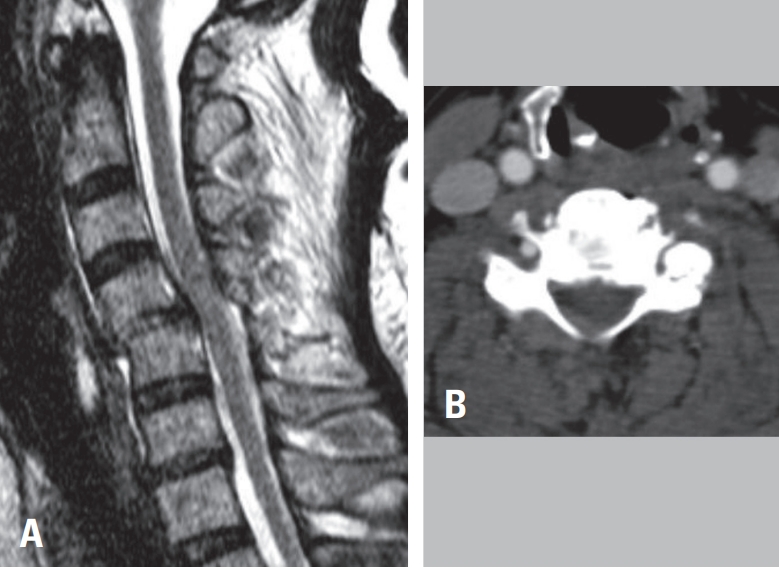
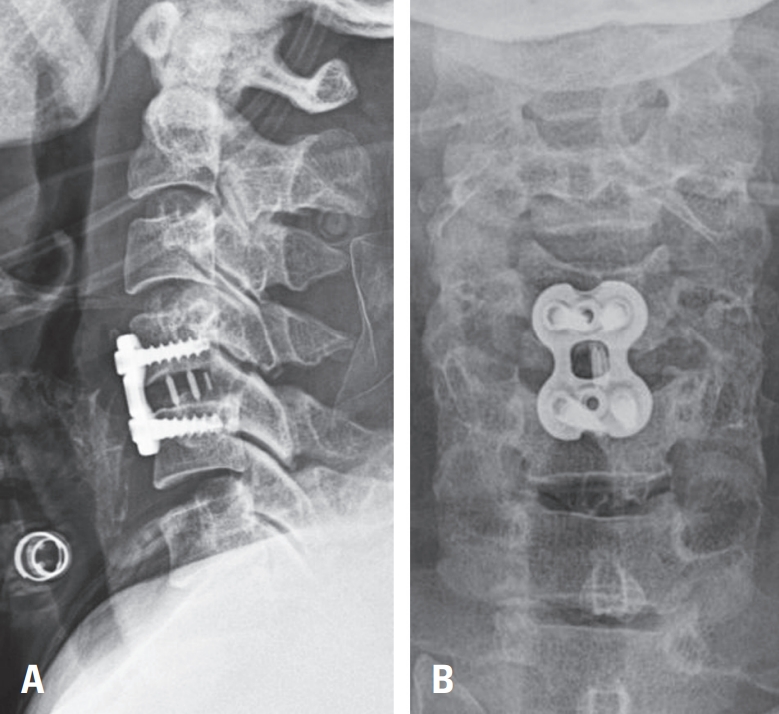
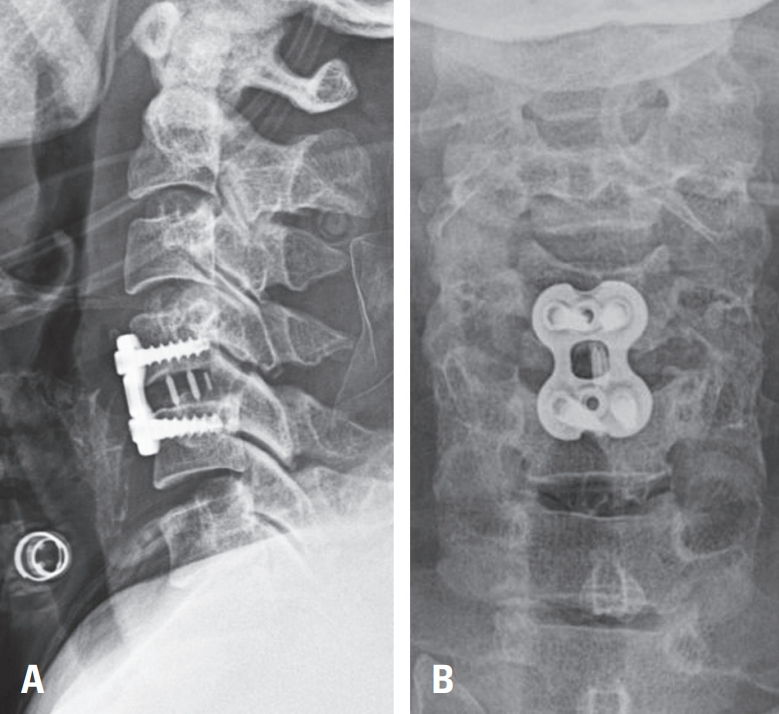
Fig. 1D). As there were no acute posterior circulation symptoms, the patient underwent urgent anterior cervical discectomy and fusion (ACDF) at C4–C5 to relieve cord compression (
Fig. 2A,
B).
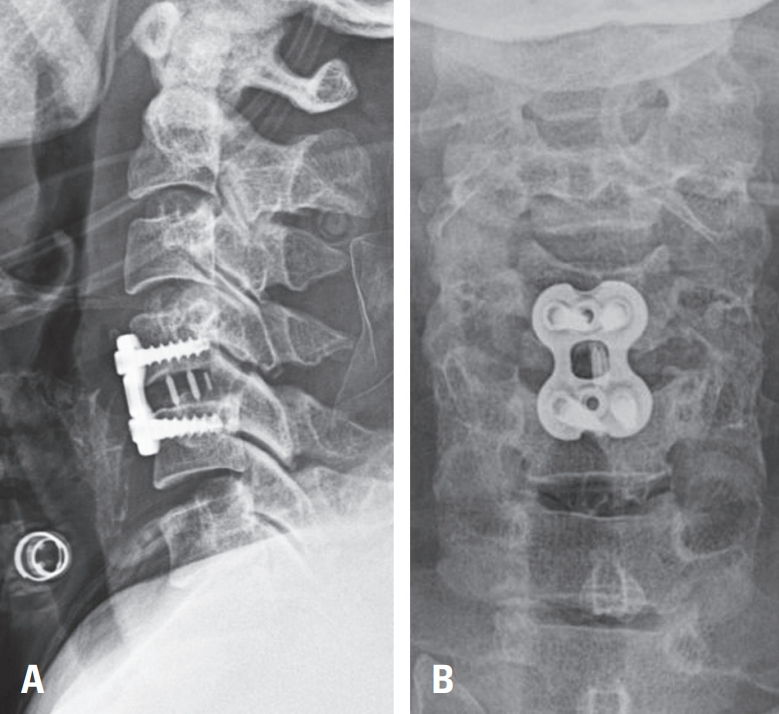
Postoperatively, her upper limb strength improved to 4/5 bilaterally, and sensory deficits resolved. Twelve hours after surgery, she developed new left facial numbness. Repeat neurologic examination showed right arm strength of 4/5 and near-intact strength on the left. Given the known vertebral artery occlusion, an urgent brain MRI was obtained; diffusion-weighted imaging revealed a high-signal lesion in the left lateral medulla (
Fig. 3A), and MR angiography demonstrated dissection-related occlusion of the left vertebral artery (
Fig. 3B). Aspirin therapy was initiated in consultation with the neurovascular team.
On postoperative day 2, she complained of severe left occipital headache. That afternoon, she reported subjective weakness of the left lower extremity and displayed gait ataxia with a leftward veer. Her previously restored left arm strength declined to 3/5. Considering her overall status, no additional endovascular procedures were performed. The patient was transferred to the department of physical medicine and rehabilitation for continued care.
At one-month follow-up, she was discharged with left arm strength recovered to 4/5, although gait ataxia persisted.
Discussion
Opalski syndrome is a rare variant of lateral medullary (Wallenberg) syndrome characterized by the addition of ipsilateral hemiparesis to the classic medullary signs of trigeminal sensory loss, dysphagia, dysarthria, and Horner’s syndrome. While most reported cases arise from spontaneous vertebral artery occlusion or dissection, post-traumatic occurrences are exceptionally rare.
1) Our case represents such an uncommon presentation following C4–C5 facet dislocation with subsequent vertebral artery dissection.
1. Pathophysiology of traumatic opalski syndrome
facet dislocation at C4–C5 imparted a shearing force to the adjacent vertebral artery, resulting in vessel wall dissection and luminal occlusion. Urgent anterior cervical decompression successfully relieved spinal cord compression and restored perfusion to the injured cord, but it did not address the dissected vertebral artery. Over the next 12 to 48 hours, the patient developed delayed lateral medullary infarction—most likely due to thromboembolic propagation from the injured segment or local reperfusion injury within the lateral medullary territory. This biphasic course underscores that surgical decompression of the spinal cord and management of vertebral artery injury represent distinct therapeutic priorities, and that vigilance for evolving brainstem ischemia must continue even after adequate cord decompression and reduction of dislocated facet joint.
2. Atypical clinical course
unlike Brown–Séquard syndrome or isolated nerveroot injury—where ipsilateral deficits follow a predictable anatomic pattern—our patient exhibited pure ipsilateral hemiparesis without contralateral spinothalamic sensory loss. Moreover, her neurological signs emerged in a biphasic fashion: initial postoperative improvement of limb strength was followed by new facial numbness at 12 hours and lower limb weakness with gait ataxia at 48 hours. This temporal dissociation highlights the potential for evolving brainstem ischemia, rather than immediate compression, in cases of traumatic vertebral artery injury.
3. Therapeutic Considerations
The management of vertebral artery dissection after recent spine surgery poses an antithrombotic dilemma. In our patient, aspirin monotherapy was initiated once medullary infarction was confirmed, while thrombolysis was deemed too high-risk given her fresh ACDF. Although intravenous thrombolysis has been reported to yield rapid improvement in spontaneous vertebral artery dissection, its safety and efficacy in the immediate postoperative setting remain undefined.
2)
4. Comparison with Spontaneous Dissection
Spontaneous Opalski syndrome most often occurs in the setting of atherosclerosis or hypertension and typically presents acutely—within minutes to hours—after vessel injury.
3) Those patients frequently experience rapid neurological recovery following intravenous thrombolysis. In contrast, our patient’s syndrome arose from traumatic shear at C4–C5 due to facet dislocation, manifested in a delayed fashion 12 to 48 hours after surgery, and achieved only partial recovery with aspirin therapy. Furthermore, unlike spontaneous cases where spinal cord injury is absent, our patient’s neurological picture was complicated by a concomitant cervical cord lesion.
5. Clinical and Research Implications
This case expands the etiologic spectrum of Opalski syndrome to include traumatic vertebral artery dissection. It emphasizes that in cervical spine trauma with facet dislocation, even in the absence of immediate posterior circulation symptoms, clinicians should remain vigilant for delayed brainstem ischemia. We propose that any new or worsening cranial nerve or limb deficits after decompression warrant prompt brainstem imaging. Finally, this report underscores the need for prospective studies to establish evidence-based antithrombotic guidelines in the postoperative management of vertebral artery dissection.
Conclusions
We report a rare case of Opalski syndrome following traumatic C4–C5 facet dislocation and vertebral artery dissection. This case underscores the potential for delayed lateral medullary infarction after cervical spine trauma and highlights the importance of early brainstem imaging and tailored antithrombotic management in such patients.
Fig. 1.
(A) Lateral cervical spine radiograph demonstrating traumatic anterior translation at C4–C5. (B) Cervical spine CT showing left C4–C5 facet dislocation. (C) Cervical spine MRI revealing spinal cord signal change at the C4–C5 level. (D) Neck CT angiography demonstrating occlusion of the left vertebral artery at C4–C5 secondary to facet dislocation.
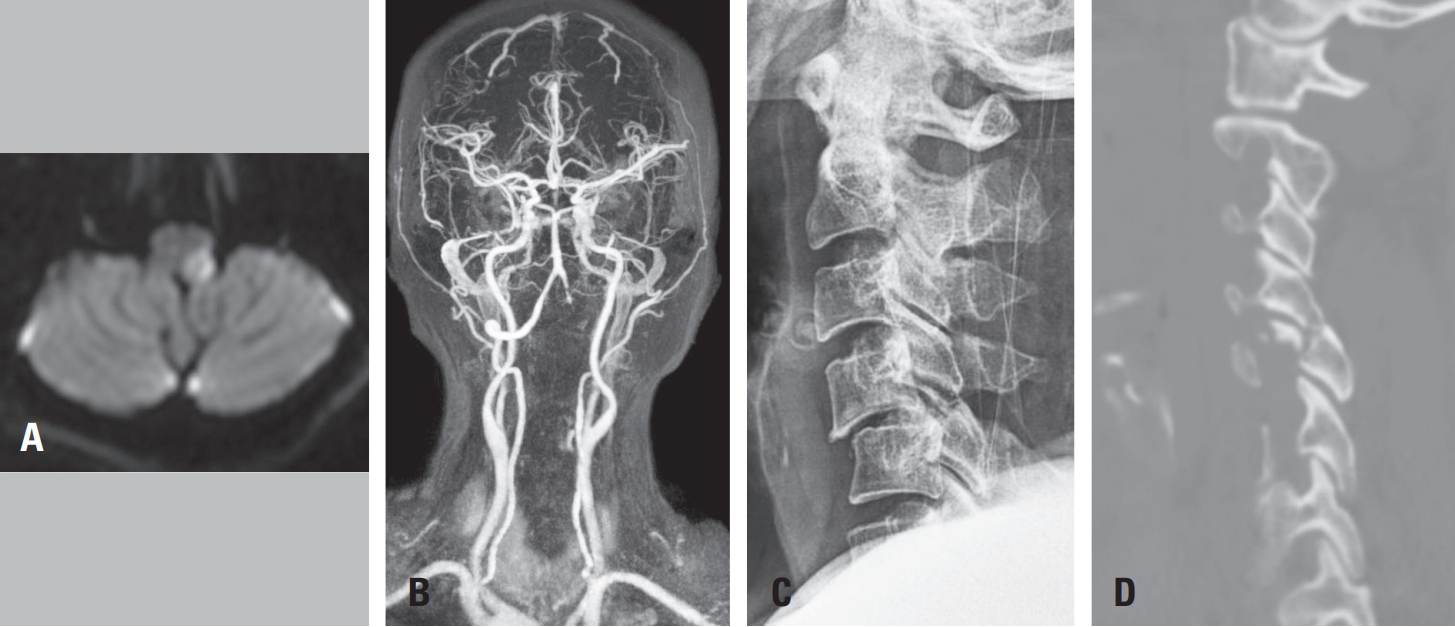
Fig. 2.
(A, B) Postoperative cervical spine radiographs (anteroposterior and lateral views) demonstrating anterior cervical discectomy and fusion (ACDF) at C4–C5.
Fig. 3.
(A) Diffusion-weighted MRI showing acute infarction in the left lateral medulla. (B) MR angiography confirming occlusion of the left vertebral artery.
References
- 1. Rukerd MRZ, Mirkamali H, Alizadeh SD. Opalski syndrome: A comprehensive systematic review of cases. Clin Neurol Neurosurg. 2024;245:108474.
- 2. Yang Y, Wang Q, Zhang S, Li J, Tang Y. Unilateral upper cervical cord infarction in Opalski’s syndrome caused by spontaneous vertebral artery dissection. Clin Med (Lond). 2023;23(4):425-6.
- 3. Hara D, Akamatsu M, Mizudami H, et al. Opalski Syndrome Treated with Intravenous Recombinant Tissue Type Plasminogen Activator-Case Report and Review of Literature. J Stroke Cerebrovasc Dis. 2020;29(8):104806.
Citations
Citations to this article as recorded by