Abstract
Osteoid osteoma is a benign bone-forming tumor that commonly affects young adults and often presents with severe nocturnal pain responsive to NSAIDs. While surgical resection is curative, lesions located in the spine, particularly near critical structures such as the vertebral artery and spinal cord, pose substantial diagnostic and surgical challenges. We report a case of a 24-year-old male with intractable night pain caused by an osteoid osteoma located at the superior margin of the right T1 pedicle. Despite extended NSAID therapy, the patient’s symptoms persisted. Multimodal imaging including MRI, CT, and PET-CT confirmed the diagnosis and revealed the lesion’s proximity to vital neurovascular structures. To minimize morbidity, we employed intraoperative O-arm navigation integrated with preoperative imaging to achieve precise localization and targeted resection through a limited posterior approach. The nidus was successfully excised en bloc without complications. Postoperatively, the patient experienced immediate pain relief and returned to normal activities within days. This case highlights the utility of real-time 3D navigation in managing spinal osteoid osteomas and supports its use as a safe, effective alternative to traditional wide exposure techniques, particularly in anatomically constrained regions of the spine.
-
Keywords: Osteoid osteoma, Spine, O-arm navigation, Minimally invasive surgery, Thoracic spine
Abstract
골양성골종(osteoid osteoma)은 주로 청소년과 젊은 성인에게 발생하는 양성 골형성 종양으로, 야간 통증과 NSAIDs에 대한 특이적인 반응을 보이는 것이 특징이다. 하지만 척추, 특히 상부 흉추와 같은 해부학적으로 민감한 부위에 발생할 경우 진단과 치료 모두에 어려움이 따른다. 24세 남성이 4개월간 지속되는 야간 상부 흉추 통증을 호소하였다. MRI, CT, PET-CT 등의 정밀 영상 검사 결과, 우측 T1 척추궁의 상연에 골양성골종이 확인되었고, 이는 추골동맥과 척수에 인접해 있어 광범위한 절개 및 척추 고정이 필요할 수 있는 위치였다. 이에 O-arm 기반 3D 내비게이션 수술을 통해 최소 절개로 병변을 정확히 위치 지정하고, 병소(nidus)를 완전 절제하였다. 수술 후 즉각적인 통증 완화가 있었으며 합병증 없이 회복되었다. 본 증례는 척추, 특히 해부학적으로 수술이 어려운 위치에 발생한 골양성골종에서도 O-arm 기반의 내비게이션 시스템을 활용하면 최소침습적이고 안전한 병소 절제가 가능함을 보여준다. 이는 전통적인 광범위 절개술을 대체할 수 있는 효과적인 수술 전략으로, 향후 척추 내 종양 수술에서 널리 활용될 수 있을 것이다.
-
색인 단어: 골양성골종, 척추, O-arm 내비게이션, 최소침습 수술, 흉추
Introduction
Osteoid osteoma is a benign osteogenic tumor that typically affects adolescents and young adults, most commonly in the second and third decades of life. It accounts for approximately 10–12% of all benign bone tumors and less than 3% of all primary bone neoplasms.
2) Histologically, the lesion is defined by a central nidus composed of osteoid and immature woven bone surrounded by a highly vascular connective tissue stroma, often embedded within a zone of dense sclerotic bone.
4) This architecture leads to a characteristic radiologic appearance and explains many of its clinical manifestations. The classic symptom is intense nocturnal pain, often described as deep, aching, or stabbing, which is remarkably responsive to nonsteroidal anti-inflammatory drugs (NSAIDs). This symptomatology is largely attributed to the overproduction of prostaglandin E2 (PGE2) by the nidus, which is known to be up to 1,000 times the concentration found in normal bone tissue.
3) While many cases are effectively managed with conservative NSAID therapy, persistent or debilitating pain often necessitates definitive treatment through complete resection of the nidus5. Although osteoid osteomas most commonly arise in the diaphysis of long bones such as the femur or tibia, approximately 10–20% of cases occur in the spine, where the posterior elements—particularly the pedicles and laminae—are preferentially involved. The presentation of spinal osteoid osteomas can be more variable and insidious. In addition to axial nocturnal pain, patients may present with painful scoliosis, nerve root irritation, or even signs of spinal cord compression depending on the lesion’s location1. The diagnosis of spinal osteoid osteoma is often delayed due to its nonspecific symptoms and subtle findings on plain radiographs. Advanced imaging modalities are essential in the diagnostic process. Thin-slice computed tomography (CT) remains the gold standard for nidus identification, given its superior resolution of cortical bone and its ability to detect the central radiolucent nidus with surrounding sclerosis6. Magnetic resonance imaging (MRI) is often used adjunctively to assess associated bone marrow edema or neural involvement but may not reliably visualize the nidus. In more diagnostically ambiguous cases, positron emission tomography-computed tomography (PET-CT) or bone scintigraphy can assist in localizing metabolically active lesions. Surgical management remains the definitive treatment in cases refractory to medical therapy. Traditionally, en bloc resection or curettage of the nidus has been performed through wide surgical exposure, including laminectomy, facetectomy, or even spinal instrumentation in certain cases. However, such approaches can result in iatrogenic instability and prolonged recovery, particularly in young patients. More recently, percutaneous techniques such as radiofrequency ablation (RFA) have been used with success in peripheral lesions but are generally contraindicated in spinal osteoid osteomas due to the risk of thermal injury to neural structures.
7) To overcome these challenges, intraoperative navigation technologies such as O-arm–based 3D imaging have been increasingly adopted. These systems provide real-time, multiplanar visualization and allow precise localization of small lesions, thereby enabling targeted bone resection with minimal disruption of surrounding anatomy. In anatomically complex regions like the cervicothoracic junction, where the vertebral artery, spinal cord, and narrow pedicles limit the surgical field, O-arm navigation has proven especially valuable. This case report highlights the successful use of O-arm navigation in a 24-year-old male with an osteoid osteoma of the superior T1 pedicle. This rare anatomic location—close to both the vertebral artery and spinal cord—would have required wide exposure and potential fusion using traditional techniques. However, with the aid of intraoperative navigation fused with preoperative CT, MRI, and PET-CT, a selective resection was performed with excellent clinical outcome. Through this case, we aim to demonstrate how advanced image-guided surgery can improve safety, accuracy, and postoperative recovery in the management of spinal osteoid osteomas.
Case Report
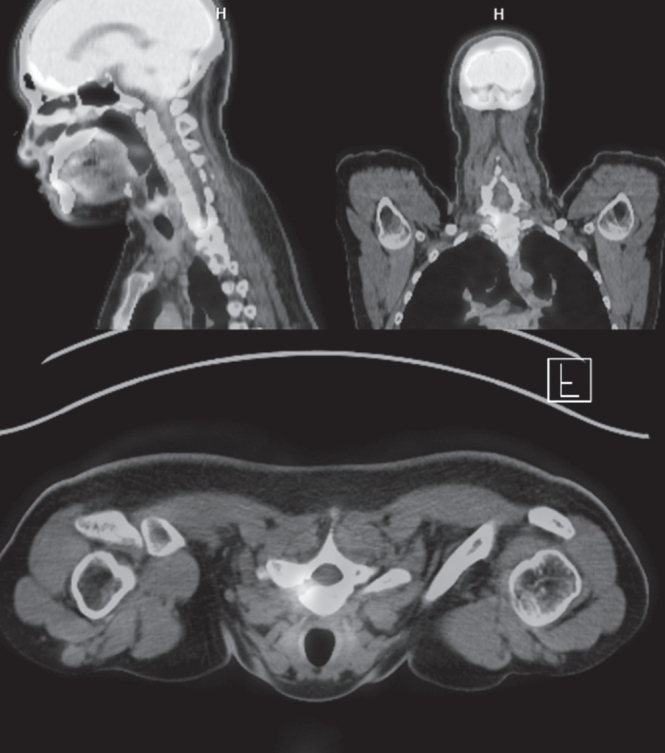
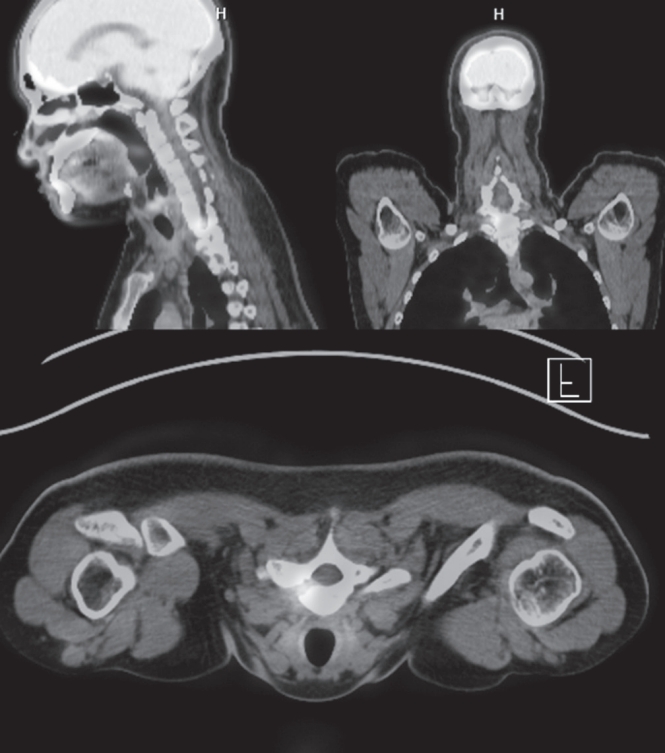
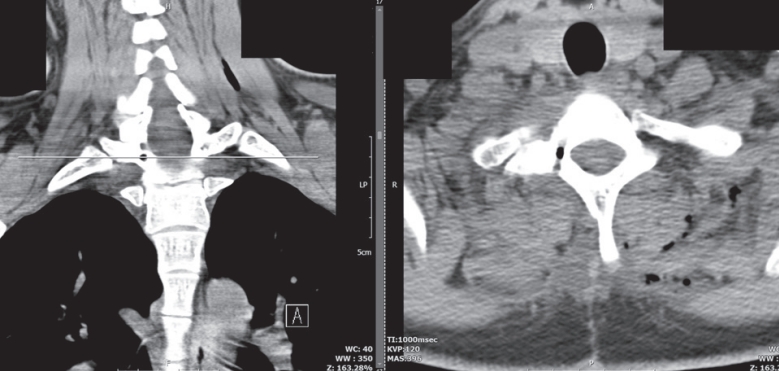
A 24-year-old otherwise healthy male presented with a 4-month history of progressively worsening right-sided upper thoracic and lower cervical pain. The pain was described as deep, dull, and aching in nature, with abrupt nocturnal onset that severely interfered with sleep. He reported frequent nighttime awakenings due to pain, unresponsive to rest or changes in posture. There was no preceding trauma, infection, or history of systemic disease. Initial self-medication with over-the-counter ibuprofen (200 mg, as needed) yielded minimal symptom relief. Upon visiting a local clinic, he was prescribed naproxen 500 mg twice daily for 14 days. As the pain persisted, celecoxib 200 mg twice daily was administered for 3 weeks, followed by etoricoxib 90 mg once daily for an additional 4 weeks. Despite good compliance, the nocturnal pain remained refractory, and his quality of life progressively deteriorated. Neurological examination was unremarkable. There were no signs of motor weakness, sensory changes, hyperreflexia, or upper motor neuron signs. No spinal tenderness or palpable mass was noted. Laboratory investigations, including ESR, CRP, and WBC count, were within normal limits. Given the persistence of symptoms despite aggressive NSAID therapy, advanced imaging was initiated. MRI of the cervicothoracic junction revealed a small lesion involving the superior aspect of the right T1 pedicle. The lesion showed hypointensity on T1-weighted images and central gadolinium enhancement on fat-suppressed T1 post-contrast sequences, surrounded by marrow edema extending into the adjacent vertebral body and lamina. Notably, the lesion appeared to abut the transverse foramen, raising concern for proximity to the vertebral artery. CT imaging demonstrated a well-defined, cortically based radiolucent nidus measuring approximately 1.2 cm, surrounded by dense reactive sclerosis—radiologically characteristic of osteoid osteoma. PET-CT further revealed focally increased FDG uptake in the nidus, indicating active bone turnover and confirming the metabolic activity of the lesion (
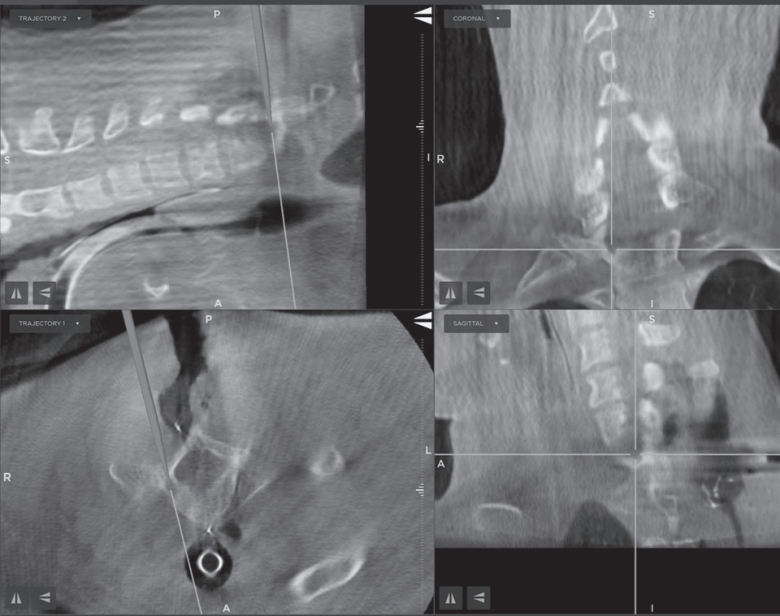
Fig. 1). Given the deep anatomical location, adjacent to both the spinal canal and the vertebral artery, wide laminectomy or facetectomy was deemed excessively invasive and potentially morbid. After a multidisciplinary team discussion, the surgical plan involved targeted resection using intraoperative O-arm–based 3D navigation to maximize precision and minimize exposure. Under general anesthesia, the patient was placed in a prone position. A midline posterior cervical incision was made, and subperiosteal dissection was carried out to expose the posterior elements of C7 and T1 on the right side. Intraoperative O-arm 3D imaging was obtained and registered with preoperative CT and MRI data using a StealthStation
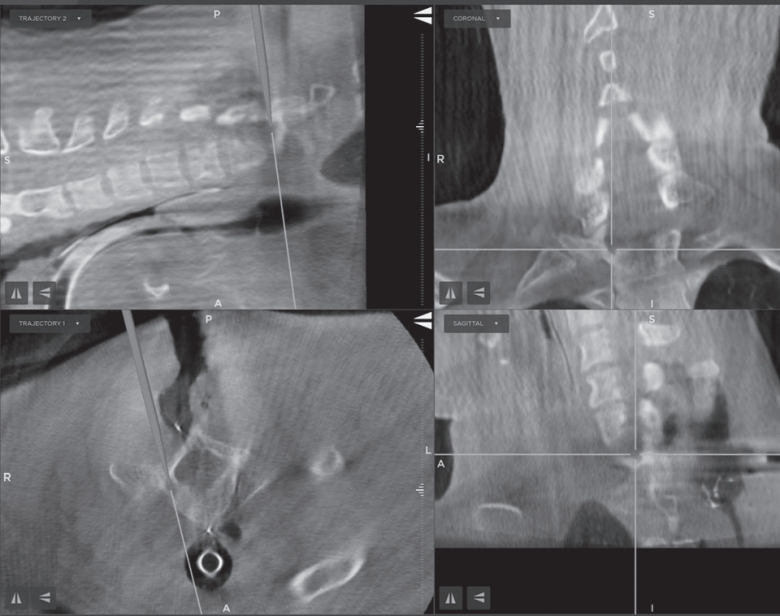
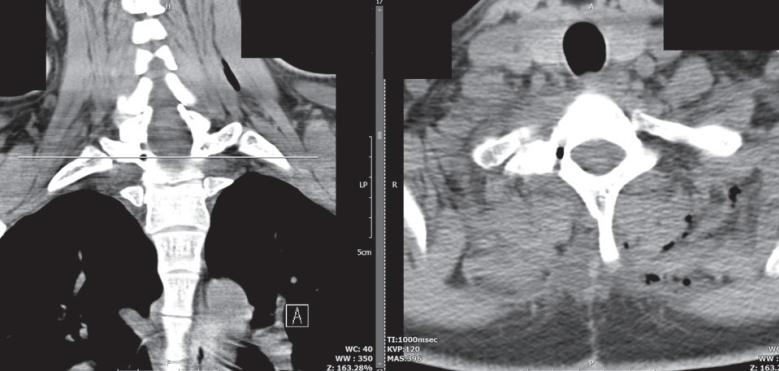
TM navigation platform (Medtronic Inc., USA). The lesion was accurately localized at the junction between the superior pedicular cortex and the transverse process of T1, just inferior to the transverse foramen (
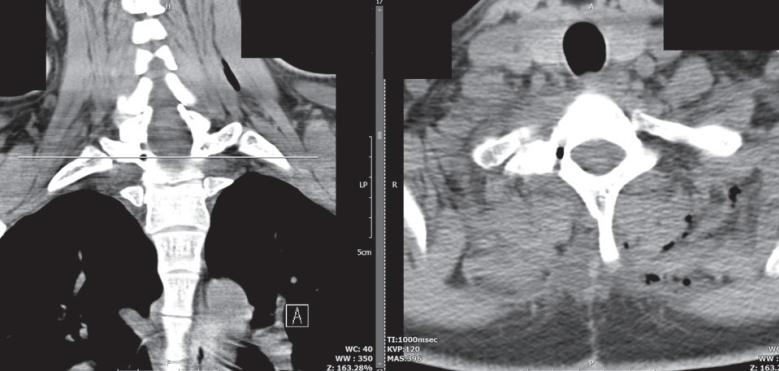
Fig. 2). Using the navigation pointer, the surgical entry point was planned to avoid disruption of the vertebral artery and facet complex. A high-speed diamond burr was used under microscopic magnification to perform a cortical window. The nidus was identified as a red-brown, well-circumscribed lesion with minimal surrounding bleeding. Complete en bloc resection of the nidus was achieved using curettes and a Kerrison punch. Care was taken to avoid injury to the transverse foramen, and no neural structures were exposed or manipulated during the procedure. Histopathological examination of the excised specimen revealed a well-vascularized nidus composed of woven bone trabeculae rimmed by active osteoblasts, consistent with osteoid osteoma. There was no evidence of malignancy. The patient experienced complete resolution of pain on the first postoperative night. No neurological complications occurred. He was mobilized without restriction on postoperative day 1 and discharged on day 2. At 6-week follow-up, he remained pain-free, had resumed full physical activity, and reported significant improvement in sleep quality. At the 6-month follow-up, repeat MRI and CT showed no evidence of recurrence or residual lesion (
Fig. 3). This case demonstrates that with accurate localization and minimal access, complete nidus resection of spinal osteoid osteomas can be achieved safely, even in anatomically high-risk areas such as the cervicothoracic junction.
Discussion
Osteoid osteoma, while benign in nature, poses significant clinical challenges when located in the spine. The deep anatomical positioning, small lesion size, and nonspecific presenting symptoms often lead to delays in diagnosis. In our case, despite classical features such as nocturnal pain responsive to NSAIDs, the spinal location made initial detection difficult on plain radiographs. This underscores the importance of cross-sectional imaging—especially CT and MRI—for accurate localization. CT, in particular, remains the gold standard for identifying the radiolucent nidus surrounded by reactive sclerosis, a hallmark of this lesion.
2) MRI, while useful for assessing perilesional edema and adjacent neural involvement, may not always clearly delineate the nidus, especially in sclerotic variants. In this case, multimodal imaging including PET-CT provided functional confirmation of lesion activity, which was particularly valuable for surgical planning. This layered diagnostic strategy is increasingly advocated in the literature for spinal lesions where conventional modalities may yield equivocal results.
4) Traditionally, complete surgical excision has been the definitive treatment for spinal osteoid osteomas that fail medical management. However, standard open surgical techniques—such as laminectomy or extensive curettage—can destabilize the spine, particularly when facet joints or pedicles are violated. In young patients, this often necessitates additional fusion, with its attendant risks and long-term biomechanical implications3. Percutaneous techniques such as CT-guided radiofrequency ablation (RFA) have shown high success rates for appendicular osteoid osteomas but are not typically recommended for spinal lesions due to the close proximity to neural structures and the risk of thermal injury.
5) Moreover, in regions like the upper thoracic spine where space is limited and the vertebral artery lies adjacent the nidus, the margin for error is minimal. Recent technological advancements—especially intraoperative 3D imaging systems like the O-arm—have revolutionized surgical management in such scenarios. These systems allow the surgeon to acquire real-time, high-resolution 3D images intraoperatively, which can be fused with preoperative MRI or CT scans. This enhances spatial orientation, facilitates precise targeting, and minimizes the extent of bony resection required to achieve complete nidus removal.
1) In our case, O-arm–assisted navigation was instrumental in localizing a nidus situated at the superior margin of the T1 pedicle, in close proximity to the vertebral artery and spinal canal. Without the benefit of intraoperative imaging, such a lesion would have necessitated a more aggressive surgical approach with significantly higher morbidity. The ability to confirm lesion location intraoperatively not only increased the confidence of the surgeon but also allowed a focused cortical window to be created, avoiding unnecessary laminectomy, facetectomy, or instrumented fusion. Several studies have echoed the advantages of image-guided minimally invasive surgery for spinal osteoid osteomas. Scarone et al. reported that intraoperative O-arm guidance significantly improved resection accuracy and reduced operative morbidity in spinal tumor cases.
6) Similarly, El-Sayed et al. demonstrated reduced recurrence rates and faster postoperative recovery when spinal osteoid osteomas were resected using computer- assisted navigation. Importantly, the complete resolution of pain in our patient immediately after surgery, coupled with the absence of complications and early return to daily activity, supports the growing consensus that image-guided, limited-access surgery offers outcomes equivalent to or better than traditional open approaches—with significantly less morbidity.
7) This case is particularly noteworthy due to the rare anatomical location of the lesion at the superior T1 pedicle, a region where surgical access is inherently difficult due to overlying shoulder girdle structures and proximity to neurovascular landmarks. The successful outcome of this case not only reaffirms the safety and efficacy of navigation-assisted resection but also supports a paradigm shift in spinal tumor surgery—moving away from wide exposure and toward precise, image-guided targeting.
Conclusions
Osteoid osteoma of the spine, particularly in anatomically constrained regions such as the cervicothoracic junction, presents significant diagnostic and surgical challenges. This case illustrates that with the integration of intraoperative O-arm navigation and multimodal preoperative imaging, precise and minimally invasive resection of spinal osteoid osteomas is not only feasible but also highly effective. By avoiding wide exposure and preserving critical anatomical structures, navigation-assisted surgery offers a safer and less morbid alternative to traditional techniques. Surgeons should consider adopting this approach in select cases where surgical precision is paramount and anatomical access is limited. As demonstrated in this report, the combination of cutting-edge imaging and careful surgical planning can result in excellent clinical outcomes—even in the most technically demanding scenarios.
Fig. 1.Preoperative PET-CT scan showing increased FDG uptake at the superior margin of the right T1 pedicle. The lesion is metabolically active and consistent with osteoid osteoma.
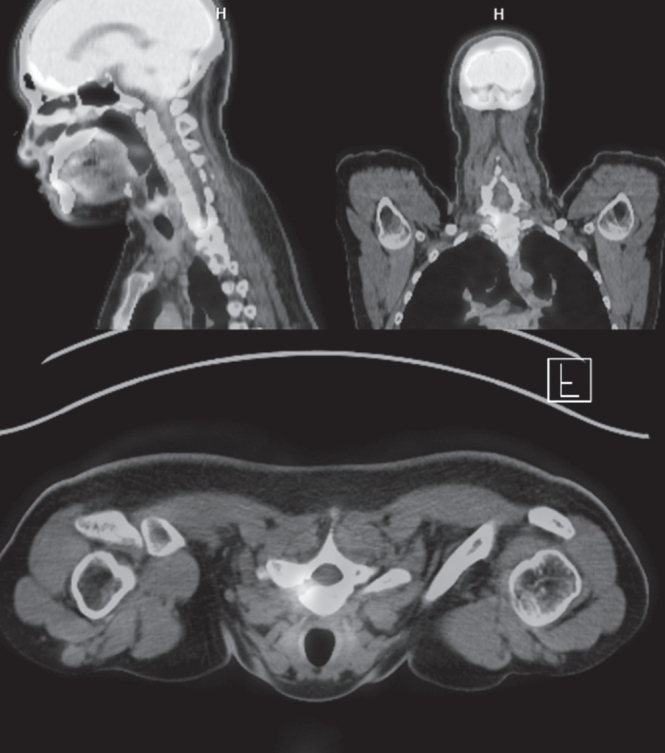
Fig. 2.Intraoperative O-arm–based navigation image demonstrating real-time localization of the nidus during surgery. The navigation pointer is positioned over the superior cortex of the right T1 pedicle.
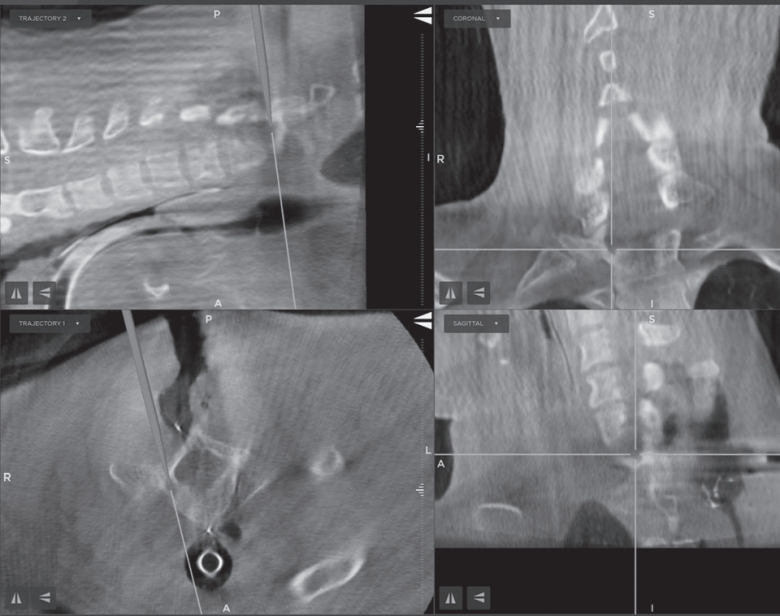
Fig. 3.Postoperative axial CT image confirming complete excision of the osteoid osteoma. The cortical window created for nidus removal is visible, with no evidence of residual lesion.
References
- 1. Cohen MD, Harrington TM, Ginsburg WW. Osteoid osteoma: 95 cases and a review of the literature. Semin Arthritis Rheum. 1983;12:265-81.
- 2. Garcia RA, Inwards CY, Unni KK:. Benign bone tumors--recent developments. Semin Diagn Pathol. 2011;28:73-85.
- 3. Greco F, Tamburrelli F, Ciabattoni G. Prostaglandins in osteoid osteoma. Int Orthop. 1991;15:35-7.
- 4. Greenspan A. Benign bone-forming lesions: osteoma, osteoid osteoma, and osteoblastoma. Clinical, imaging, pathologic, and differential considerations. Skeletal Radiol. 1993;22:485-500.
- 5. Kneisl JS, Simon MA. Medical management compared with operative treatment for osteoid-osteoma. J Bone Joint Surg Am. 1992;74:179-85.
- 6. Rosenthal DI, Springfield DS, Gebhardt MC, Rosenberg AE, Mankin HJ. Osteoid osteoma: percutaneous radiofrequency ablation. Radiology. 1995;197:451-4.
- 7. Tanaka M, Sonawane S, Uotani K, Fujiwara Y, Sessumpun K, Yamauchi T, et al. Percutaneous C-Arm Free OArm Navigated Biopsy for Spinal Pathologies: A Technical Note. Diagnostics (Basel). 11:2021.
Figure & Data
Citations
Citations to this article as recorded by