| Si-Young Park | 5 Articles |
Osteoid osteoma is a benign bone-forming tumor that commonly affects young adults and often presents with severe nocturnal pain responsive to NSAIDs. While surgical resection is curative, lesions located in the spine, particularly near critical structures such as the vertebral artery and spinal cord, pose substantial diagnostic and surgical challenges. We report a case of a 24-year-old male with intractable night pain caused by an osteoid osteoma located at the superior margin of the right T1 pedicle. Despite extended NSAID therapy, the patient’s symptoms persisted. Multimodal imaging including MRI, CT, and PET-CT confirmed the diagnosis and revealed the lesion’s proximity to vital neurovascular structures. To minimize morbidity, we employed intraoperative O-arm navigation integrated with preoperative imaging to achieve precise localization and targeted resection through a limited posterior approach. The nidus was successfully excised en bloc without complications. Postoperatively, the patient experienced immediate pain relief and returned to normal activities within days. This case highlights the utility of real-time 3D navigation in managing spinal osteoid osteomas and supports its use as a safe, effective alternative to traditional wide exposure techniques, particularly in anatomically constrained regions of the spine.
Objective
Postoperative urinary retention (POUR) is a common complication following lumbar spine surgery, significantly affecting functional recovery and Enhanced Recovery After Surgery (ERAS) protocols. POUR can lead to bladder overdistension, infections, prolonged hospital stays, and long-term detrusor dysfunction. Postoperative delirium (POD) can impair cognitive function and mobility, potentially triggering or exacerbating POUR. This study aims to investigate whether POD serves as an independent risk factor for POUR and to analyze other contributing factors to provide clinical management strategies. Materials and Methods A retrospective cohort study was conducted involving 420 patients who underwent lumbar spine surgery at a single tertiary medical institution between March 2021 and February 2024. POUR was defined as a post-void residual (PVR) bladder volume ≥300 mL measured via bladder ultrasound or requiring catheter reinsertion due to urinary retention. POD was diagnosed within 72 hours postoperatively using the Confusion Assessment Method (CAM) and was classified into three subtypes: hyperactive, hypoactive, and mixed. Multivariate logistic regression analysis was employed to identify the relationship between POD and POUR, with sensitivity and specificity assessed through Receiver Operating Characteristic (ROC) curve analysis. Results Among 420 lumbar spine surgery patients, 44 (10.5%) experienced POD. Of these, 16 (36.4%) were classified as hyperactive, 20 (45.5%) as hypoactive, and 8 (18.2%) as mixed type. POUR occurred in 28 of the POD patients (63.6%) compared to 71 of 376 patients without POD (18.9%), demonstrating a statistically significant difference (p<0.001). The analysis of POUR incidence by POD subtype revealed rates of 62.5% (10/16) for hyperactive POD, 60.0% (12/20) for hypoactive POD, and 75.0% (6/8) for mixed POD. Patients with mixed POD showed the highest POUR incidence, with a significant difference compared to hyperactive and hypoactive POD (p<0.05). Multivariate logistic regression analysis identified POD as an independent risk factor for POUR, increasing the likelihood by approximately 3.7 times (Odds Ratio, OR: 3.71; 95% Confidence Interval, CI: 1.95–7.06; p<0.001). Among POD subtypes, mixed POD presented the strongest association with POUR, increasing the risk by 4.8 times (OR: 4.84; 95% CI: 2.10–11.15; p<0.001). Hyperactive and hypoactive POD were also significant risk factors, increasing POUR risk by 3.0 times (OR: 3.04; 95% CI: 1.45–6.35; p=0.003) and 3.5 times (OR: 3.48; 95% CI: 1.69–7.19; p=0.001), respectively. Conclusions This study confirms that postoperative delirium (POD) is an independent risk factor for postoperative urinary retention (POUR) in lumbar spine surgery. The occurrence and subtype of POD significantly influence POUR incidence, with mixed POD presenting the highest risk. These findings highlight the importance of early diagnosis and prevention of POD as a strategy to effectively reduce POUR. A multidisciplinary approach integrating POD and POUR management could optimize postoperative outcomes and improve patient recovery.
Numerous improvements in minimally invasive spine surgery (MISS) have been made during the past decade.
Classic treatment methods have reserved surgical intervention for trauma patients with neurological compromises or instability. When used in thoracolumbar spine trauma management, MISS should achieve the similar results as classic treatment with less morbidity.(1) In the past decade, minimally invasive surgical (MIS) techniques for spine surgery have been increasingly used. The goal of minimally invasive surgery is to decrease surgical morbidity through decreased soft-tissue dissection providing similar structural stability as classic techniques. An increasing number of studies is reporting good clinical and radiographic outcomes with MIS techniques. However, the literature is lacking high-quality evidence comparing these newer techniques to classic treatments. In the future, development of techniques can expand the indications and treatment possibilities in spine trauma treatment. We reviewed the current literatures to clarify the indications of minimally invasive techniques with spinal trauma.
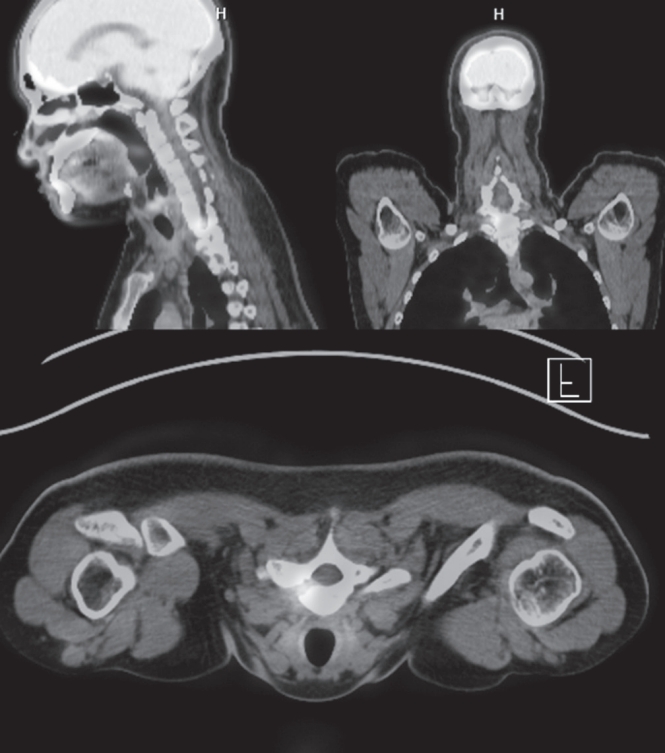
Although metastatic lung adenocarcinoma in the spinal cord is rare, it can be diagnosed by positron emission tomography and computed tomography (PET/CT) scan with high sensitivity during the early disease stage. A clinical and radiographic review was performed to present a rare case of an intradural intramedullary adenocarcinoma metastasis in the spinal cord with a negative PET/CT scan. A 75-year-old man with a diagnosis of lung cancer without metastasis confirmed by a negative PET/CT scan with no spinal symtoms (conducted 6 weeks previously) presented with progressive paralysis of both lower extremities and accompanying bowel and bladder symptoms. He underwent radical lobectomy of left lung under diagnosis of lung cancer without distant metastasis 6 weeks ago. Emergent MRI was performed, and MRI revealed a large intradural intramedullary mass compressing the spinal cord and extending from T12 to L1 with anterior compression of the spinal cord. Surgical decompression and tumor resection from T12 to L1 by lumbar laminectomy and durotomy were performed under a microscope. And, a diagnosis of adenocarcinoma to the spinal cord was made based on histopathologic findings. Postoperatively, the patient’s neurologic status was not significantly improved. Despite a negative PET/CT scan finding with no neurologic symptoms or pain, surgeons should not exclude the possibility of a spinal metastatic lesion with lung cancer.
Objectives
To evaluate the effectiveness of a prototype plate and cage device (PCB) in cervical spine disease. Summary of Background Data: Several Cage-Screw implants have recently been developed to avoid cervical platerelated complications. Methods A total of 34 patients with cervical disc protrusion who underwent PCB implantation between 2004 and 2007 were included in the study. There were 22 males and 12 females with a mean age of 49.9 years (range: 30 to 62 years). Odom’s Criteria were evaluated in all patients for a minimum follow-up period of 1 year (mean 24.6 months). Radiographic evaluation was performed to assess the status of fusion, intervertebral disc height, cervical lordosis and segmental kyphosis. Results In general, there were 20 excellent cases, 10 good cases and 4 fair cases according to Odom’s Criteria. In terms of radiological results, the height of intervertebral disc space was measured three different times, as follows: pre-operation, mean 6.07 mm; post-operation, mean 9.52 mm; last follow-up, mean 8.74 mm. No patients showed segmental instability on flexion-extension view at the last follow-up appointment. There were no cases of screw back out or device failure and no donor site morbidity. Conclusion PCB implant for degenerative cervical disease may restore intervertebral disc space and lordotic angle of the cervical spine without significant complications.
|
|

