Abstract
-
Purpose
Glomangiomas of the spine are exceptionally rare benign vascular tumors, frequently misdiagnosed as more common lesions such as schwannomas or meningiomas. Although most spinal glomangiomas exhibit benign behavior, the presence of a BRAF V600E mutations may indicate uncertain malignant potential. Accurate diagnosis and complete surgical excision are essential for favorable outcomes.
-
Methods
A 43-year-old male with left flank pain was evaluated with thoracic MRI and underwent surgical resection. Histopathological and molecular analyses were performed.
-
Results
Thoracic magnetic resonance imaging (MRI) revealed a 2.8 cm ovoid, hypervascular mass adjacent to left T10 transverse process, extending to the posterior hemithorax. Surgical resection was performed, and histopathological examination confirmed a glomangioma with positive smooth muscle actin (SMA) expression and a BRAF V600E mutation.
-
Conclusions
This case highlights the diagnostic challenge posed by paraspinal glomangiomas and emphasizes the importance of histopathological and molecular analysis in establishing the correct diagnosis. A review of the literature demonstrates that complete surgical excision remains the treatment of choice, with excellent prognosis. The identification of BRAF mutations may warrant closer follow up.
-
Keywords: Glomangioma, Glomus tumor, Spinalneoplasms, Paraspinal regions
Abstract
-
목적
척추에서 발생하는 글로만지오마(glomangioma)는 매우 드문 양성 혈관성 종양으로, 신경초종이나 수막종과 같은 보다 흔한 종양으로 오진되는 경우가 많다. 대부분의 척추 글로만지오마는 양성 경과를 보이나, BRAF V600E 돌연변이가 동반된 경우 악성 잠재성을 시사할 수 있다. 정확한 진단과 완전한 수술적 절제가 좋은 예후를 위해 중요하다.
-
대상 및 방법
좌측 옆구리 통증을 주소로 내원한 43세 남자 환자에서 흉추 자기공명영상(MRI)을 시행하였고, 종양 절제 수술을 시행하였다. 절제된 병변에 대해 병리조직학적 검사 및 분자유전학적 분석을 시행하였다.
-
결과
흉추 MRI에서 좌측 T10 횡돌기 인접 부위에서 후방 흉강으로 연장되는 2.8 cm 크기의 난원형 고혈관성 종괴가 관찰되었다. 수술적 절제를 시행하였으며, 병리조직학적 검사에서 smooth muscle actin (SMA) 양성을 보이는 글로만지오마로 진단되었고, BRAF V600E 돌연변이가 확인되었다.
-
결론
본 증례는 척추 주위(paraspinal) 글로만지오마의 진단적 어려움을 보여주며, 정확한 진단을 위해 병리조직학적 및 분자유전학적 분석이 중요함을 강조한다. 문헌 고찰 결과, 완전한 수술적 절제가 표준 치료이며 예후는 매우 양호하다. 다만 BRAF 돌연변이가 확인된 경우에는 보다 면밀한 추적 관찰이 필요할 수 있다.
-
색인 단어: 글로만지오마, 글로무스 종양, 척추 종양, 척추 주위 병변
Introduction
Glomus tumors are rare, benign mesenchymal neoplasms that originate from the glomus body.
1) While these tumors most commonly arise in the subungual regions of the hands or feet,
2) their occurrence in deep-seated locations such as the spine is exceedingly rare, with fewer than 20 cases reported in the literature to date.
3,4) Spinal glomangiomas most frequently localize to the thoracic or lumbar spine.
3) often within epidural or paravertebral spaces. Intradural extramedullary involvement is exceedingly rare, with few cases described.
5) Despite their generally benign biological behavior, spinal glomangiomas present significant diagnostic challenges due to their nonspecific clinical and radiological features. Patients commonly present with chronic pain, neurological deficits, or radicular symptoms depending on the tumor location and extent.
Herein, we report a rare case of a thoracic paraspinal glomangioma in a middle-aged male patient. Histopathological examination confirmed the diagnosis of glomangioma with a BRAF V600E mutation. This case emphasizes the diagnostic challenges associated with spinal glomangiomas and highlights the potential role of molecular analysis in guiding clinical management.
Case Presentation
A 43-year-old male with no previous medical history presented to our outpatient clinic with left flank pain for last 2 months. The pain was constant and aggravated with daily activities. There were no associated neurological symptoms. At presentation, his Japanese Orthopaedic Association (JOA) score was 15.
Physical and neurological examinations revealed no abnormalities. Laboratory findings were unremarkable.
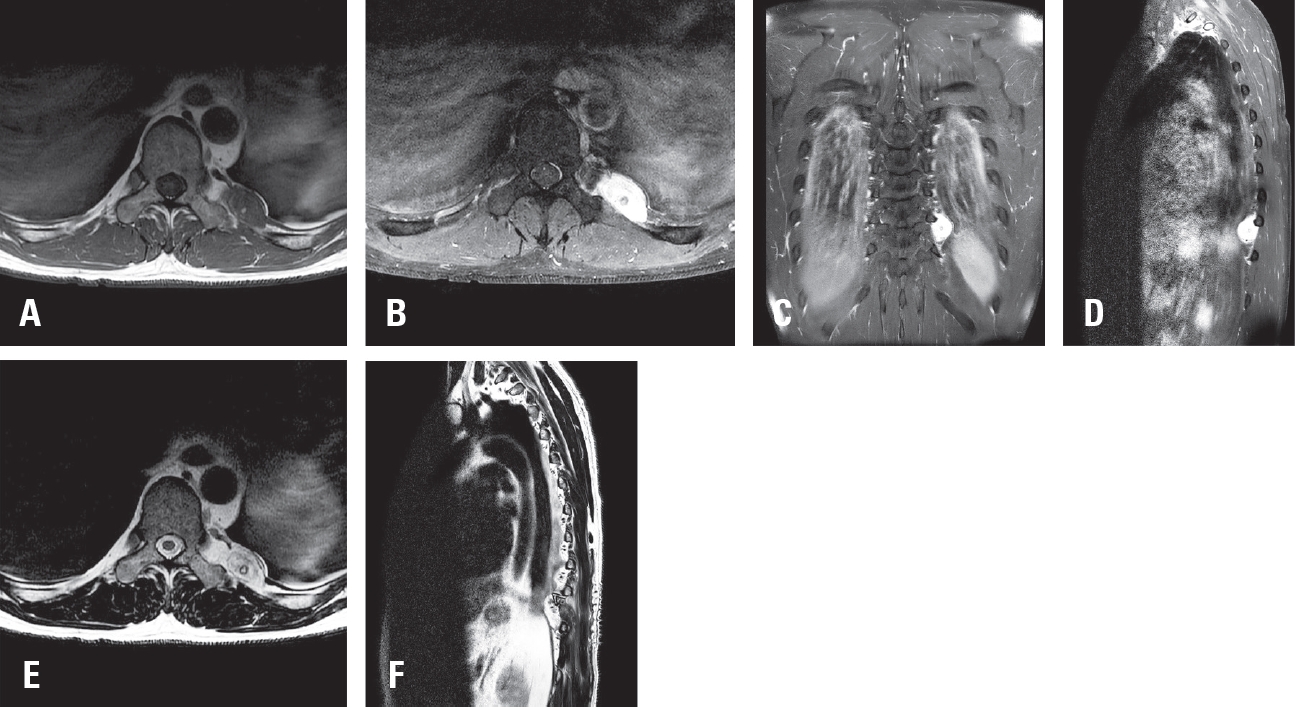
Magnetic resonance imaging (MRI) demonstrated a 2.8 cm ovoid, hypervascular mass at the T10–T11 level in the left posterior hemithorax, encasing the left 10th rib and adjacent to the left T10 transverse process. The mass showed hypointensity on T1-weighted images (
Fig. 1A), hyperintensity on T2-weighted images (
Fig. 1E,
F), and homogeneous enhancement after contrast administration (
Fig. 1B-
D). Based on these imaging characteristics, the lesion was initially suspected to be a schwannoma, and surgical resection was planned.
The patient underwent surgical excision of the mass via a paramedian approach. Intraoperatively, the tumor was located near the left 10th rib and was easily dissected from the surrounding tissues. The mass was completely removed without difficulty. No intraoperative or immediate postoperative complications were noted.
Histopathological examination revealed features consistent with glomangioma. Microscopic analysis showed a vascular proliferation composed of round to oval glomus cells with well-defined cytoplasmic borders, arranged around dilated vascular channels (
Fig. 2A,
B). Immunohistochemical staining demonstrated diffuse positivity for smooth muscle actin (
Fig. 2C) and a low proliferative index (Ki-67, 4–5%). The tumor cells were negative for S100 and STAT6. Molecular analysis and immunohistochemical staining confirmed the presence of a BRAF V600E mutation (
Fig. 2D).
Postoperatively, the patient’s left flank pain resolved completely. He was discharged in good condition without complications. Follow-up MRI confirmed complete resection of the mass with no evidence of residual tumor (
Fig. 3A,
B).
Discussion
Glomangiomas are vascular-rich benign neoplasms arising from the glomus body, a specialized arteriovenous structure involved in thermoregulation.
1) While they most commonly occur in the distal extremities, especially in subungual regions,
2) spinal or paraspinal glomangiomas are rare. A few cases of thoracic and lumbar spine are reported in the literature.
3,4)
One of the greatest challenges in managing spinal glomangiomas is the difficulty of establishing a preoperative diagnosis.
6) As demonstrated in our case, radiological features such as hypointensity on T1-weighted images, hyperintensity on T2-weighted images, and homogeneous enhancement after gadolinium administration are non-specific and frequently overlap with more common spinal tumors, including schwannomas, meningiomas, and paragangliomas.
7,8) In this case, we initially suspected a paravertebral schwannoma originating from the intercostal nerve.
Definitive diagnosis requires histopathological and immunohistochemical analysis.
9) Glomangiomas characteristically demonstrate positive staining for smooth muscle actin (SMA) and CD34, with negative staining for neural markers such as S100 and STAT6.
10) These findings help distinguish glomangiomas from other neurogenic or mesenchymal tumors that can present similarly in the paraspinal region. In our case, the tumor demonstrated positivity for SMA and CD34, while negative for S100 and STAT6. Furthermore, the Ki 67 labeling index was approximately 4–5%, supporting a low proliferative potential and favoring a benign biological behavior.
However, molecular analysis revealed the presence of a BRAF V600E mutation within the tumor. Recent studies have identified this mutation in a subset of glomus tumors, primarily those with atypical or malignant features.
11) While BRAF mutations have not been extensively studied in glomangiomas, their presence has been associated with increased mitotic activity and aggressive clinical behavior in other glomus tumor subtypes.
12) The coexistence of a low Ki 67 index and BRAF V600E positivity in our case introduces a degree of uncertainty regarding the tumor’s long-term biological behavior. Although our histopathological findings favor a benign lesion, the molecular profile suggests the need for cautious interpretation. Given limited available data, particularly regarding spinal glomangiomas, it remains unclear whether BRAF mutations carry the same prognostic significance in this tumor subtype. Nevertheless, the identification of a BRAF mutation may warrant more vigilant long-term surveillance.
Surgical resection remains the treatment of choice for spinal glomangiomas.
3) The benign nature of these tumors, along with their well circumscribed margins, often allows for complete excision. Gross total resection is associated with excellent outcomes and a low recurrence rates.
3,13) In our case, a paramedian approach facilitated safe and complete removal of the tumor, with immediate resolution of the patient’s flank pain and no postoperative complications. Follow-up MRI confirmed the absence of residual tumor. These favorable results are consistent with prior reports of spinal glomangiomas, where complete resection has been associated with excellent long-term prognosis.
In conclusion, spinal glomangiomas are rare but should be considered in the differential diagnosis of paraspinal masses, particularly when imaging suggests a hypervascular lesion.
8) Preoperative differentiation from other spinal tumors remains challenging, emphasizing the need for histopathological and molecular confirmation.
9) The detection of a BRAF V600E mutation in our case highlights the evolving role of molecular pathology in glomangioma diagnosis and raises important questions regarding prognosis and surveillance, warranting further investigation.
11)
Conclusions
Spinal glomangiomas are rare tumors that can be difficult to distinguish from other paraspinal lesions based on imaging alone. This case underscores the importance of considering glomangioma in the differential diagnosis of hypervascular paraspinal masses. Histopathological and molecular analysis, including BRAF mutation testing, play key role in confirming the diagnosis and assessing tumor behavior.
Fig. 1.Preoperative magnetic resonance imaging (MRI) of the thoracic spine. (A) Axial T1-weighted image showing a hypointense mass at the left T10–11 level. (B) Axial T1-weighted dolinium-enhanced image demonstrating homogeneous enhancement. (C) Coronal T1-weighted gadolinium-enhanced image showing the ovoid mass in the left posterior hemithorax. (D) Sagittal T1-weighted gadolinium-enhanced image delineating the extent of the mass. (E) Axial T2-weighted image showing a hyperintense lesion. (F) Sagittal T2-weighted image confirming hyperintensity of the mass.

Fig. 2.Histopathological and immunohistochemical findings of the tumor. (A) Histological analysis showing a well-circumscribed, multilobulated vascular-rich tumor surrounded by fibrous stroma. (B) Histological analysis demonstrating uniform round to oval glomus cells with eosinophilic cytoplasm, arranged around dilated vascular channels. (C) Immunohistochemical staining for smooth muscle actin (SMA) shows diffuse cytoplasmic positivity in tumor cells. (D) Immunohistochemical staining using BRAF V600E antibody shows diffuse cytoplasmic positivity in tumor cells.

Fig. 3.
Postoperative thoracic spine MRI. (A) Axial T2-weighted image showing complete resection of the previously identified mass.
(B) Sagittal T2-weighted image confirming no residual lesion.

References
- 1. Janssen KA, et al. Glomus tumors: clinical and morphologic study. J Cutan Pathol. 2012;39(3):345-50.
- 2. Gleeson M, et al. Glomus tumors of the hand: a systematic review. Hand (N Y). 2018;13(1):61-7.
- 3. Li X, Zheng J. Extradural glomus tumor of the thoracic spine: case report and review. Ann Palliat Med. 2021;10(8):9309-17.
- 4. Czyżewski W, et al. Diagnostic and therapeutic insights into spinal glomangioma: systematic review. Diseases. 2024;12(132.
- 5. Bessho Y, et al. Intraosseous glomus tumor in the upper thoracic spine: case report. Spine (Phila Pa 1976). 1991;16:988-90.
- 6. Patel NP, et al. MRI characteristics of glomus tumors. J Hand Surg Am. 2021;46(2):172.e1-2.e8.
- 7. Zhang H, et al. Spinal glomus tumor mimicking schwannoma: case report. J Spine Surg. 2021;7(3):237-42.
- 8. Kuo C-H, et al. Unusual imaging presentation of spinal glomus tumor. J Spine Surg. 2017;3:3963.
- 9. Wang C, et al. Immunohistochemical features of glomus tumors. Diagn Pathol. 2014;9:42.
- 10. Lee C, et al. Spinal paravertebral glomangioma: case report. Asian Spine J. 2017;11(2):292-6.
- 11. Karamzadeh Dashti N, et al. BRAF V600E mutations in glomus tumors. Am J Surg Pathol. 2017;41(10):1367-4.
- 12. Chakrapani A, et al. BRAF and KRAS mutations in sporadic glomus tumors. Am J Dermatopathol. 2012;34(5):533-5.
- 13. Arregui M, et al. Complete response to encorafenib plus binimetinib in a BRAF-mutant metastatic glomangiosarcoma. Oncotarget. 2024;15(1):717-24.
Citations
Citations to this article as recorded by